CASE20220529_001
Post Infaction Ventricular Septal Defect Blockage: Direct Externalization and Emneshment to Right Ventricular moderator band
By Bryan Rene Toledano, Ramon Miguel Montana Rivera, Cathleen Faye Lu, Louisa Joan Go Go, Irwin Bundalian, Michelangelo L. Sabas, Dexter Cheng
Presenter
Bryan Rene Toledano
Authors
Bryan Rene Toledano1, Ramon Miguel Montana Rivera, Cathleen Faye Lu1, Louisa Joan Go Go4, Irwin Bundalian1, Michelangelo L. Sabas1, Dexter Cheng5
Affiliation
The Medical City, Philippines1, National Children's Hospital, Philippines4, Medical city hospital, Philippines5
Structural Heart Disease - Others (Structural Heart Disease)
Post Infaction Ventricular Septal Defect Blockage: Direct Externalization and Emneshment to Right Ventricular moderator band
Bryan Rene Toledano1, Ramon Miguel Montana Rivera, Cathleen Faye Lu1, Louisa Joan Go Go4, Irwin Bundalian1, Michelangelo L. Sabas1, Dexter Cheng5
The Medical City, Philippines1, National Children's Hospital, Philippines4, Medical city hospital, Philippines5
Clinical Information
Relevant Clinical History and Physical Exam
A 70 year old female with multiple comorbidities was transfered to our institution due to hypotension and heart failure symptoms. She experienced severe chest pain 5 days prior for which no consult was done. Her blood pressure was 90/60mmHg on norepinephrine drip and 02 saturation of 95% on nasal cannula 4-5 lpm. A harsh holosystolic murmur and thrill heard best on the left sternal border and bilateral crackles on both lower lung fields were appreciated.
Relevant Test Results Prior to Catheterization
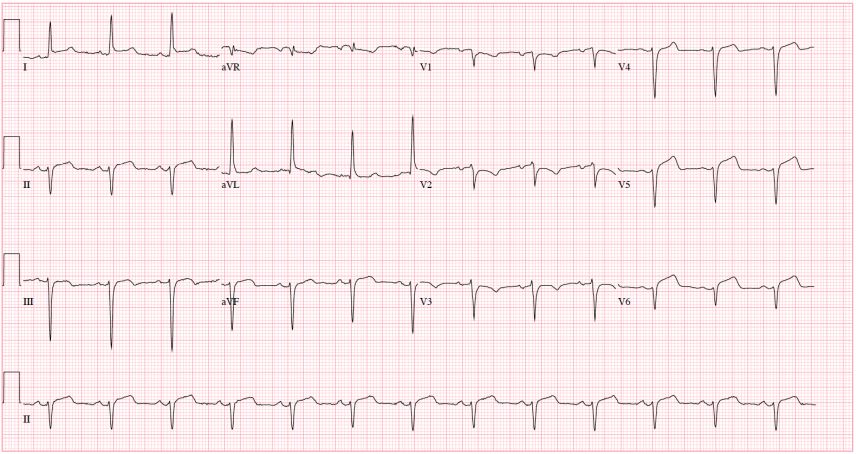
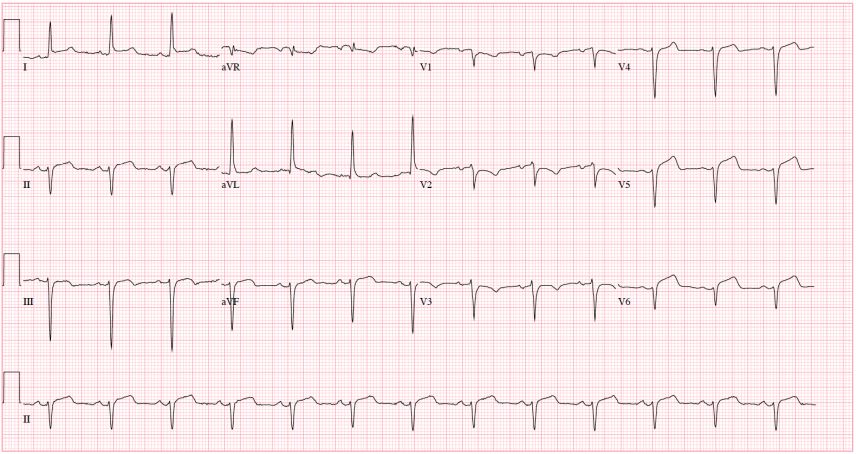
On serial 12 lead echocardiograms ST elevation in the lateral with ischemia in the anteroseptal leads but no interval changes were seen. The Troponin I was elevated at 28,310 pg/ml. Transthoracic echocardiography (TTE) showed a Left Ventricle (LV) ejection fraction of 65%, an apical regional contraction abnormality with mild Right Ventricular (RV) dysfunction. Bubble study showed negative contrast effect in the RV secondary to apical Post Infarction Ventricular Septal Defect (PIVSD)
 4C bubble study.mp4
4C bubble study.mp4
Relevant Catheterization Findings
Coronary angiography showed a distal occlusion of the LAD and non obstructive lesions in other coronaries. She was referred to surgery for PIVSD repair and revascularization. Her condition quickly deteriorated, on the 4th day of hospitalization she was intubated, and on triple vasopressors. Serial TTE showed an enlarging apical PIVSD 1.8-2.1 cm, Qp/Qs >3:1, swiss cheese appearance on color doppler, aneurysmal LV, moderate RV dysfunction and severe tricuspid regurgitation (TR)

 Apical VSD.mov
Apical VSD.mov
 A4C with color TR.mp4
A4C with color TR.mp4

Interventional Management
Procedural Step
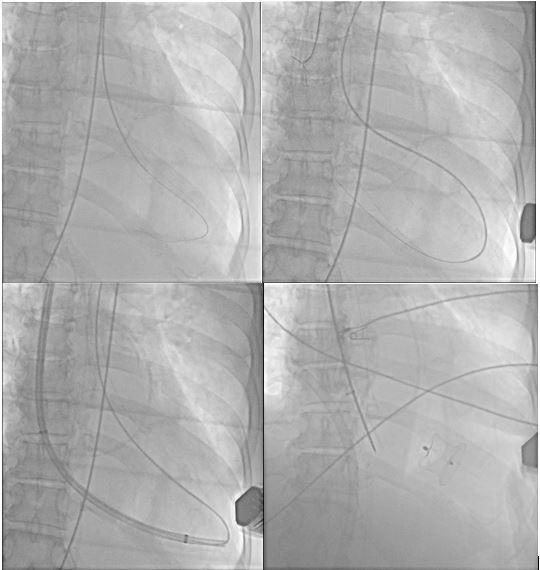
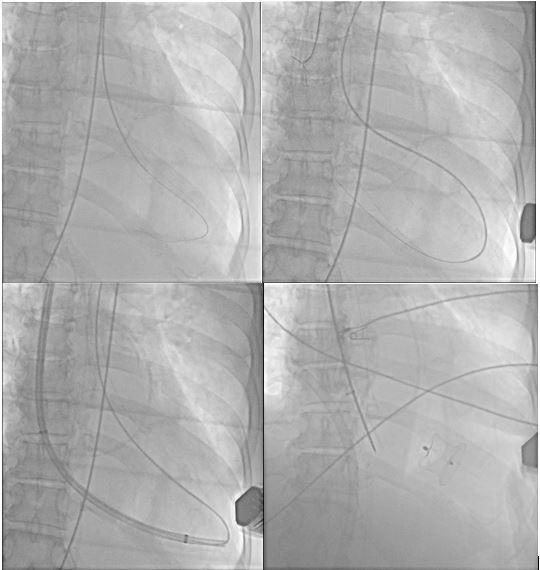
The procedure was performed in the catheterization laboratory under general anesthesia, TTE and fluoroscopic guidance. Using TTE, the RV Moderator Band (MB) diameter in the apex was measured at 15mm. The right Femoral Artery (FA) and right Internal Jugular Vein (IJV) were accessed with a 5F and 14F introducer sheaths respectively. Using 5F JR4 catheter over a 0.035' 260cm glidewire in the FA, the aortic valve, LV and apical PIVSD were directly crossed. The glidewire was snared in the right atrium via the IJV and externalized to create an ArterioVenous (AV) loop. The system was used to track and position the 12F delivery sheath across the RV MB, PIVSD and parked in the LV. A Patent Ductus Arteriosus (PDA) 26 x 24mm occluder device, followed at the sheath tip and was partially opened, as the AV loop is broken. The sheath and device assembly were pulled into the apical PIVSD and furthermore to enmesh with the RV MB where it was fully deployed. There was sudden improvement of blood pressure and discontinuation of vasopressors. The Pulmonary Artery pressure dropped from 68/37 mmHg to 35/17mmHg. TTE showed a small residual shunt, improved RV function and resolution of TR. The device was temporarily left attached for prevention of inadvertent embolization
 Post Dexter procedure.mp4
Post Dexter procedure.mp4
 3D rendered mod band money with device.mp4
3D rendered mod band money with device.mp4
Case Summary
In a large, complex, apical PIVSD with no inferior rims, direct exerternalization and enmeshment to right ventricular moderator band (DEXTER) concept allows for exclusion of the defect and vestigialization of the RV apex. An immediate and dramatic hemodynamic improvements can be achieved.
